A patient is receiving cefazolin in combination with anticoagulants, a practice that requires careful consideration due to potential drug interactions and the need for close monitoring. This article provides a comprehensive overview of cefazolin and anticoagulants, including their mechanisms of action, potential interactions, monitoring strategies, and management considerations.
Cefazolin is a cephalosporin antibiotic commonly used to treat various bacterial infections. Anticoagulants, on the other hand, are medications that prevent or reduce blood clotting. When these two classes of medications are combined, it is essential to understand their potential interactions and the appropriate management strategies to ensure patient safety and optimize therapeutic outcomes.
Cefazolin and Anticoagulants
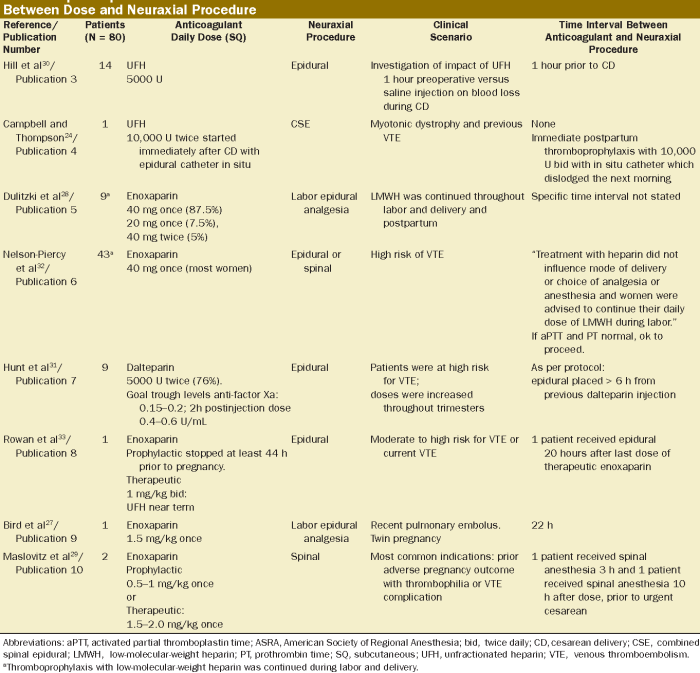
Cefazolin is a cephalosporin antibiotic that inhibits bacterial cell wall synthesis. It is commonly used to treat infections caused by susceptible bacteria, such as Staphylococcus aureusand Streptococcus pneumoniae. Anticoagulants, on the other hand, are medications that prevent or reduce blood clotting. They are often used to prevent or treat conditions such as deep vein thrombosis (DVT) and pulmonary embolism (PE).
Types of Anticoagulants
There are different types of anticoagulants, each with its own mechanism of action:
- Heparin:A naturally occurring anticoagulant that inhibits thrombin, a key enzyme in the coagulation cascade.
- Warfarin:An oral anticoagulant that inhibits vitamin K-dependent clotting factors (II, VII, IX, and X).
- Direct oral anticoagulants (DOACs):A class of newer oral anticoagulants that directly target specific clotting factors, such as factor Xa (e.g., rivaroxaban, apixaban) or thrombin (e.g., dabigatran).
Potential Drug Interactions
Cefazolin can interact with anticoagulants, increasing the risk of bleeding. This is because cefazolin can interfere with the metabolism of warfarin, leading to increased warfarin levels in the blood. DOACs, on the other hand, do not interact with cefazolin in the same way.
Monitoring and Management
Importance of Monitoring Coagulation Parameters, A patient is receiving cefazolin in combination with anticoagulants
During cefazolin therapy, it is important to monitor coagulation parameters to assess the risk of bleeding. This is especially important in patients receiving anticoagulants, as the combination of these medications can increase the risk of bleeding complications.
Frequency of Coagulation Testing
The recommended frequency of coagulation testing during cefazolin therapy depends on the type of anticoagulant being used:
| Anticoagulant | Frequency of Testing |
|---|---|
| Heparin | Daily or more frequently if the patient is unstable |
| Warfarin | Weekly or more frequently if the patient’s INR is unstable |
| DOACs | No routine testing is required |
Management of Abnormal Coagulation Results
If abnormal coagulation results are detected, the following management strategies may be considered:
- Hold cefazolin:If the patient is experiencing active bleeding or has a significantly elevated INR, cefazolin should be held until the bleeding is controlled or the INR is normalized.
- Adjust anticoagulant dose:The dose of the anticoagulant may need to be reduced if the patient is experiencing excessive bleeding.
- Transfusion of fresh frozen plasma:In cases of severe bleeding, transfusion of fresh frozen plasma may be necessary to correct coagulation abnormalities.
Special Considerations
Patient Populations Requiring Extra Caution
Certain patient populations require extra caution when receiving cefazolin with anticoagulants due to an increased risk of bleeding. These populations include:
- Patients with a history of bleeding disorders
- Patients with severe liver or kidney disease
- Patients taking other medications that increase the risk of bleeding (e.g., aspirin, non-steroidal anti-inflammatory drugs)
Alternative Antibiotics or Anticoagulants
In patients who are at high risk of bleeding, alternative antibiotics or anticoagulants may be considered. For example, vancomycin may be used instead of cefazolin, and low-molecular-weight heparin (LMWH) may be used instead of warfarin.
Patient Education and Counseling
Key Points for Patient Counseling
Patients receiving cefazolin with anticoagulants should be counseled on the following key points:
- The importance of adhering to the prescribed medication regimen
- The signs and symptoms of bleeding and what to do if they occur
- The importance of avoiding activities that increase the risk of bleeding (e.g., contact sports)
- The need to inform their healthcare provider of any other medications they are taking
FAQ Overview: A Patient Is Receiving Cefazolin In Combination With Anticoagulants
What are the potential drug interactions between cefazolin and anticoagulants?
Cefazolin can increase the anticoagulant effect of warfarin, leading to an increased risk of bleeding. Therefore, it is essential to monitor coagulation parameters closely and adjust warfarin dosage accordingly.
How often should coagulation parameters be monitored during cefazolin therapy?
The frequency of coagulation testing depends on the patient’s individual risk factors and the type of anticoagulant being used. Generally, coagulation parameters should be monitored at baseline, then daily for the first few days of therapy, and then less frequently as the patient stabilizes.
What are the appropriate management strategies for patients with abnormal coagulation results?
If a patient develops abnormal coagulation results, the healthcare professional should assess the patient’s clinical status, adjust the anticoagulant dosage or type as necessary, and monitor the patient closely for any signs of bleeding or thrombosis.